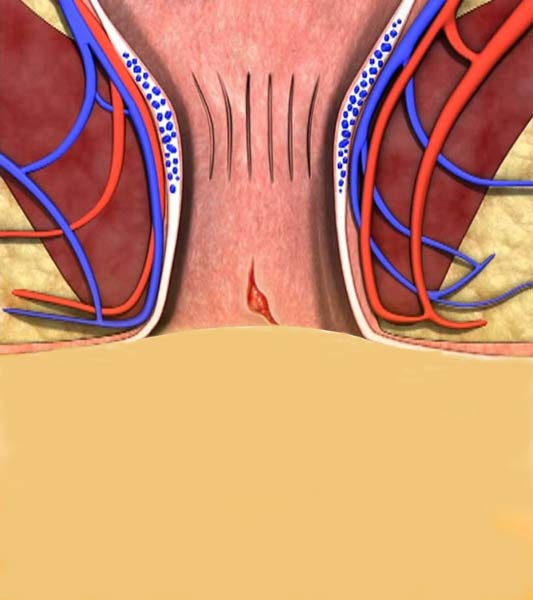
Fissure is a linear prolate lysis of the sequence of the mucosa of the lower third of the anal canal from the dentate line to the lip of the anus.
It is a common condition that occurs at all ages with the same frequency in both sexes. It is distinguished into acute when the symptoms last less than 6 weeks and chronic when the symptoms last more than 6 weeks. Acute fissure is superficial while when it is chronic there is a deep ulcerative lesion with affected lateral walls that show hardening. The chronic one is accompanied by a hypertrophic fold (sentinel tag) at the lower end of the fissure and the hypertrophic anal valve (anal nipple i) which can develop into fibrous polyp at the upper end. In 90% of cases it is located behind the midline (6th hour) while anterior fissure (12th hour) is observed in 10% of cases mainly in women.
Despite extensive investigation of the disease, the exact etiology remains unclear. Any injury to the end of the anal canal can cause fissure. Constipation is usually blamed where hard stools injure the mucosa, however fissure is less common in patients with diarrhea. Studies have shown that dysfunction (hypertonicity-spasm) of the internal sphincter and reduced blood flow (ischemia) in the anal canal play a role in the creation of fissure.
The symptoms are severe pain during defecation or immediately after, bleeding and itching (itch). Fissure is the most common cause of proctalgia and the symptoms can cause a significant reduction in the patient's quality of life.
Most patients can be treated conservatively. Conservative measures include high fluid intake, a high-fiber diet, oral laxatives, avoidance of paper, and finally lukewarm anus baths that reduce pain and spasm of the internal sphincter and improve blood circulation. Conservative treatment also includes ointments that have analgesic effects and ointments that relax the internal anal sphincter (ointments containing nitroglycerin or calcium emulators).
Another method of treating fissure is the injection of botox (botulismotoxin) locally under inebriation, with the aim of temporal relaxation of the internal sphincter which is hypertonic, in order to heal the fissure with a success rate of 60-70%. Botulismotoxin acts as an inhibitory neurotransmitter by preventing the release of acetylcholine from nerve endings. The main side effect is moderate gas and faecal incontinence that lasts for about 3 weeks.
Unfortunately, conservative treatment often fails, especially in cases of chronic fissure. In these cases but also when there is very intense pain, surgery is required. There are several surgical methods:
- Internal lateral sphincterotomy which is considered the treatment of choice for the treatment of fissure with a success rate of 90-98%. The operation eliminates the spasm, facilitates healing and prevents recurrence. Side effect of the method is incontinence at a rate of 2-11%.
- Fissure removal with laser or electrodiathermia without sphincter damage with very good results and without the risk of incontinence.
- Surgical resection of the fissure with the surrounding fibrous tissue and repair of the deficit with a good bloody flap.
The surgeries are performed under brief general or regional anesthesia (spinal, epidural) and the patient is discharged the same day.
 English
English  Ελληνικά
Ελληνικά