Hemorrhoids have been known since antiquity. Etymologically the word hemorrhoid consists of the Greek words "blood" and "flow", which describe exactly the symptom of blood loss.
They are usually characterized by bleeding from the rectum during defecation, on the stool, with or without prolapse of a tissue in the anal area.
It is a fact that the patient often describes as "hemorrhoids" anything that he locates or bothers him in the anal area. Of course, the diagnosis is of primary importance, as different pathological conditions in the anus have different treatment as well as different prognosis and importance.
What are hemorrhoids?
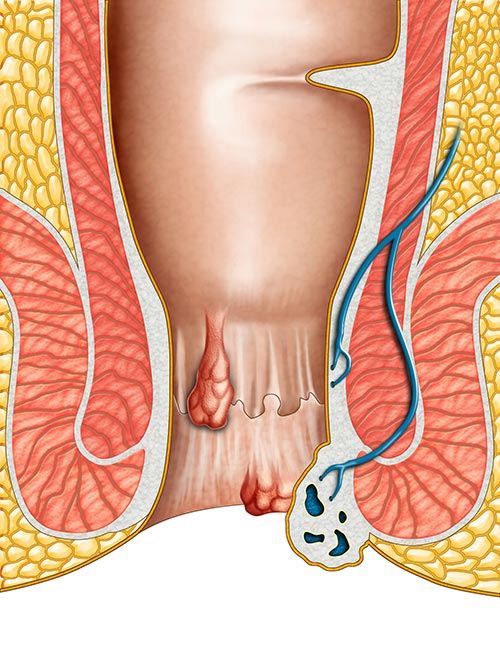
The prevailing view until now, that hemorrhoids are dilated veins, is not accurate. Hemorrhoids are a pathological term that describes the symptomatic and abnormally downward displacement of anal tissues (anal pad). The specific anatomical formations - anal pad - are located in the lower part of the large intestine and in the anus, circularly. These anatomical structures are present under normal conditions in all people and contribute to the mechanism of abstinence, i.e. to better seal the anus and to control cenoses. This displacement results from the destruction of the supporting connective tissue and the abnormal circulation of blood within these tissues, with the result that these moving tissues cause dilation and deformation of the hemorrhoid plexus.
Therefore, normal hemorrhoids are not a disease but part of our body. However, when the hemorrhoids are irritated, swollen and prolapsed, they cause unpleasant symptoms for the patient and then we use the term “hemorrhoidopathy”. In our daily life when we say I have hemorrhoids, we mean that I have pathological hemorrhoids.
Cause
Hemorrhoidopathy is a disease that manifests itself at an unsuspected time and in a very large percentage of the population. The cause of hemorrhoidopathy is unknown, but the factors that seem to predispose and increase the risk of hemorrhoidopathy are the following:
- Chronic constipation
- Pregnancy / childbirth
- Heavy work that contributes to the frequent increase in intra-abdominal pressure
- Hereditary predisposition
- Sedentary lifestyle and obesity
- Prolonged standing
- Inadequate hygiene of the anal area
Hemorrhoids - Can They Be Prevented?
The best prevention for hemorrhoids is to keep the stool soft to facilitate their elimination and intestine cenocis without much effort, as soon as possible after the need arises. Exercise, walking and eating a diet high in fiber and fluids help reduce constipation by softening stools and facilitating their elimination.
Diagnosis and classification of hemorrhoids
The most common symptom of hemorrhoids is painless anal bleeding during defecation, which may be accompanied by prolapse of anal tissue. Usually, blood does not mix with the stool but surrounds the outer surface of the stool or is seen during cleansing after defecation. The main feature of blood is its light red color, as the hemorrhoid plexus is directly connected to the vascular network. Patients with complicated hemorrhoids (i.e. external hemorrhoids with acute thrombosis and strangulated internal hemorrhoids) may experience anal pain and lumps at the tip of the anus. On the other hand, patients with simple hemorrhoids usually do not have any anal pain.
In daily practice, acute anal pain is more likely to occur due to anal fissures and rectal abscesses.
In order to diagnose hemorrhoids it is imperative to have an accurate history and detailed medical examination, which will include a finger examination of the anus and proctoscopy. Even if no light-colored blood has appeared, every patient with anal bleeding should have a sigmoidoscopy or colonoscopy, especially those at risk for colon cancer.
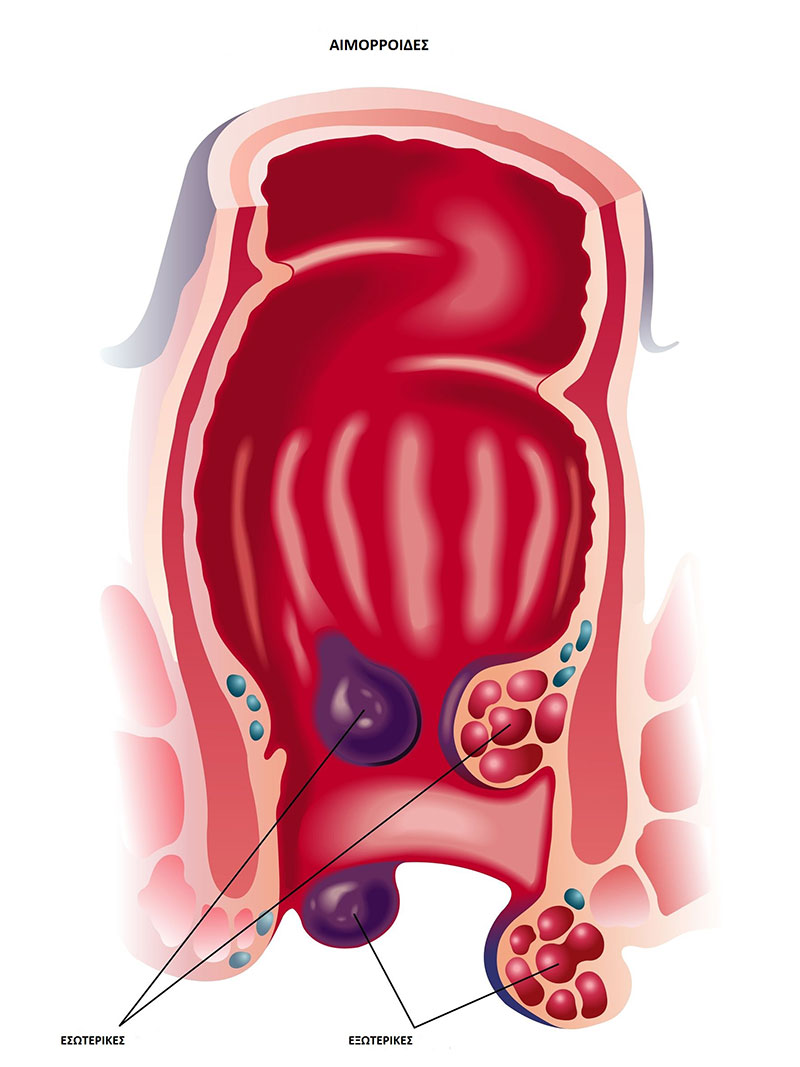
Hemorrhoids are generally classified according to their location. They are divided into internal, which appear above the dentate line of the anus and are covered by intestinal mucosa, to external, which are located below the dentate line and are covered by skin and in mixed ones.
Internal hemorrhoids are further classified according to their appearance and degree of prolapse:
In the 1st stage the hemorrhoids are visible only with the proctoscope and are manifested with little blood loss.
In the 2nd stage belong those hemorrhoids which in the cenosis periodically and not always prolapse but are reduced on their own.
In the 3rd stage, hemorrhoids prolapse during defecation but are reduced only by hand. Generally at this stage they cause less blood loss than those of the 2nd stage but more often a feeling of intolerance in the anus. At this stage there is always the risk of thrombosis and constriction.
In the 4th stage the hemorrhoids are permanently out of the anus and cannot be reduced. They cause mucus to leak out, which can cause dermatitis and itching in the area.
Four stages in the prograssion of hemorrhoidopathy.
Treatment
Treatment options depend mainly on the type, kind and location of hemorrhoids.
Hemorrhoids do not require any specific treatment unless they present with recurrent bleeding, acute thrombosis or discomfort to the patient. Stage 1 and 2 hemorrhoids can be effectively treated with changes in diet and lifestyle and with medication.
Sclerotherapy involves injecting a sclerosing substance such as phenol into the hemorrhoid. In this way the veins shrink and the hemorrhoids contract.
Cauterization methods have been shown to be effective for hemorrhoids and are used when other conservative methods fail: electrocauterization, infrared radiation, laser surgery or cryosurgery.
Hemorrhoid ligation with an elastic ring (hemorrhoid fasciation) is a method in which elastic rings are applied to internal hemorrhoids at least 1 cm above the dentated line to stop perfusion.
Classic hemorrhoidectomy (Milligan-Morgan), which can also be done with the use of ultrasound, has very good and permanent results. Also Longo hemorrhoidectomy (hemorrhoid coagulation) is applied in recent years with very good results and the advantage of the patient's rapid return to daily activities. It is a procedure that involves removing a ring of abnormally enlarged hemorrhoidal tissue and repositioning the rest of the hemorrhoidal tissue in its normal anatomical position with a special machine (circular anastomosis)
Ultrasound-guided ligation of the H.A.L. hemorrhoidal arteries is an innovative, minimally invasive method. A special tool locates the branches of the lower hemorrhoidal artery with the help of ultrasound. After locating them, they are ligated with absorbable sutures. This reduces the perfusion of the hemorrhoidal plexus and consequently the internal pressure, resulting in the shrinkage of the hemorrhoids to their original size.
In recent years, with the new dual-wavelength laser diodes, the treatment of hemorrhoids of all degrees is painless and effective with a cure rate of over 90% and with the patient leaving the clinic after a few hours.
Hybrid Hemorrhoidoplasty is designed individually for each patient. Hemorrhoids are not the same in all patients and the treatment must take into account age, chronicity of the problem, lifestyle and work. Its success is based on the simultaneous application of several, minimally invasive, state-of-the-art techniques, depending on the nature and extent of the problem.
The method ensures the definitive solution to the problem of hemorrhoids in a quick and effective way, without complications, without pain, without discomfort and offers immediate recovery and return of the patient to his daily activities.
 English
English  Ελληνικά
Ελληνικά