Kondylomas are the symptom of a human papilloma virus (HPV) virus infection.
Kondyloma virus infection is the most common sexually transmitted disease. It is estimated that 50-70% of sexually active men and women will be infected with the HPV virus in their lifetime.
It is estimated that in any sexual contact with an infected person without precaution there is a 70% risk of infection with the virus. However, kondylomas will occur in only 10% of those who become infected, as in most cases the kondyloma virus is treated by the immune system and remains dormant.
There are over 130 types of the virus and some are low risk while some are high risk. Low-risk types of the HPV virus (6, 11, 42, 43, 44, 54, 61, 70, 72, 81) usually cause benign lesions, the most well-known of which are condyloma acuminatum. Virus types 6 and 11 are responsible for about 90% of these lesions. High-risk types of the HPV virus (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73, 82) can, under appropriate conditions, cause the development of various types of cancer in the body, such as the cervix, vagina, vulva, anus, penis and oropharynx.
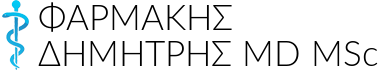
Condylomas acuminatum are small tumors - small skin lesions shaped like a small cauliflower (anthracnose). They can be flat or protruding from the skin, small as a pinhead or larger, single or multiple. They usually have an abnormal surface and their color is red-pink or gray-cinereal, they have a flattened base or a stem, while their texture is soft.
Condylomas are usually visible to the naked eye, however, sometimes they are not visible on plain visual examination and the doctor needs to use a more specific examination, colposcopy or proctoscopy. In women they appear on the skin of the vulva, vagina, cervix, perineal skin, anal ring and rectal mucosa. In men they usually appear on the penis or urethra, testicles, anal ring and rectal mucosa. Finally, in both women and men they can also appear in the mouth.
SYMPTOMS-DIAGNOSIS
Condylomas usually have no symptoms. The patient perceives them by touch or sees them with a magnifying glass. Depending on their size and anatomical position, they may be accompanied by pain or itching (itch). In rare cases they can cause bleeding or ulcers. If the codylomas are external, the doctor can see them and identify them either by examining the area or using a special apparatus, the colposcope or with the proctoscope, if they are located in the anus. But if they are internal, they can be suspected from the result of the Pap test. With colposcopy or proctoscopy biopsies can also be taken to confirm the diagnosis. Finally, the evolution of diagnostic tests is the molecular standardization techniques of the HPV type. The polymerase chain reaction (PCR) method detects the DNA of the condyloma virus and we can standardize the virus.
HOW THEY ARE TRANSMITTED
Codylomas are transmitted mainly through sexual intercourse, even with incomplete sex, which is why they are classified as Sexually Transmitted Diseases (STDs). If one sexual partner has condylomas acuminatum, it is easy to transmit them to the other. If the skin or mucous membranes (mucosa = membrane covering internal cavities, such as the mucous membranes of the mouth and vagina) are rubbed against the skin or mucous membranes of an infected person, the partner may become infected with the virus. They are also transmitted from mother to fetus during normal childbirth. For this reason, when condylomas are present, a caesarean section is recommended.
Using a condom reduces the chance of transmission, but not completely, as only the areas that come in contact with the condom are protected.
HOW THEY ARE TREATED
From the moment the diagnosis is made, the doctor, depending on the problem that exists, will suggest the appropriate solutions. The methods of treatment of condylomas acuminatum are divided into pharmaceutical and surgical. Medications include podophyllotoxin and imiquimod, which are administered by the patient himself and trichloroacetic acid and podophyllin, which are applied by the doctor. Surgical methods include the destruction of condylomas by cryocoagulation, electrodiathermy and laser and the removal (resection) of condylomas.
CAN THEY COME BACK?
Treatment is not always effective and relapses are observed. Once a person becomes infected with the virus, he remains a carrier and there is a small chance that the virus will recur after treatment. In this case, the treatment should be repeated. In general, however, it is good to remember that recurrences of lesions are few and that they usually occur within the first year of their appearance.
Factors that favor their recurrence
- Inadequate hygiene - care of the genital area
- diabetes mellitus
- immunodeficiencies and immunosuppressants
- not using a condom
- lack of good sleep and healthy diet and smoking
- topical use of ointments containing corticosteroids.
FREQUENTLY ASKED QUESTIONS
- What about the HPV vaccine?
In our country it is considered that the best age group for HPV vaccination is 12-14 years old (before the start of sexual intercourse). It is also indicated for older women, up to the age of 26 and is provided free of charge by the insurance funds of our country. It is recommended by all global health organizations.
- Can condylomas affect fertility?
Many women ask whether condylomas can influence and affect their fertility. The answer is that, under normal circumstances, condylomas do not affect a woman or a man's fertility. Of course, what they can cause is a temporary infertility, due to the emotional stress created by their diagnosis and the consequent psychological upset and possibly the temporary reduction of sexual mood.
- Are condylomas transmitted through oral sex?
According to the latest scientific data, the HPV virus can be transmitted through oral contact (oral sex), especially if there are small scratches - loosening of the skin or mucous membranes in the relevant areas.
 English
English  Ελληνικά
Ελληνικά