Thyroid cancer can occur at any age. Most cases manifest after the age of 40. Women are two to three times more likely to get the disease than men. When there is a family history of thyroid cancer, the risk of developing the disease in other family members is higher.
People who have been exposed to radiation to the throat area have a significantly higher risk of developing the disease. Ionizing radiation is a major cause of thyroid cancer.
In the case of the Chernobyl nuclear accident, the radioactive substances released into the environment, particularly radioactive iodine, were absorbed by the body of the people in the area where the accident took place. Children absorbed much more radioactive iodine due to their development, resulting in a dramatic increase in thyroid cancer in children and adolescents in the affected areas after the accident.
Patients who have received radiation therapy for cancer of the head, throat or thorax are more likely to develop this cancer because the thyroid gland was in the radiation field.
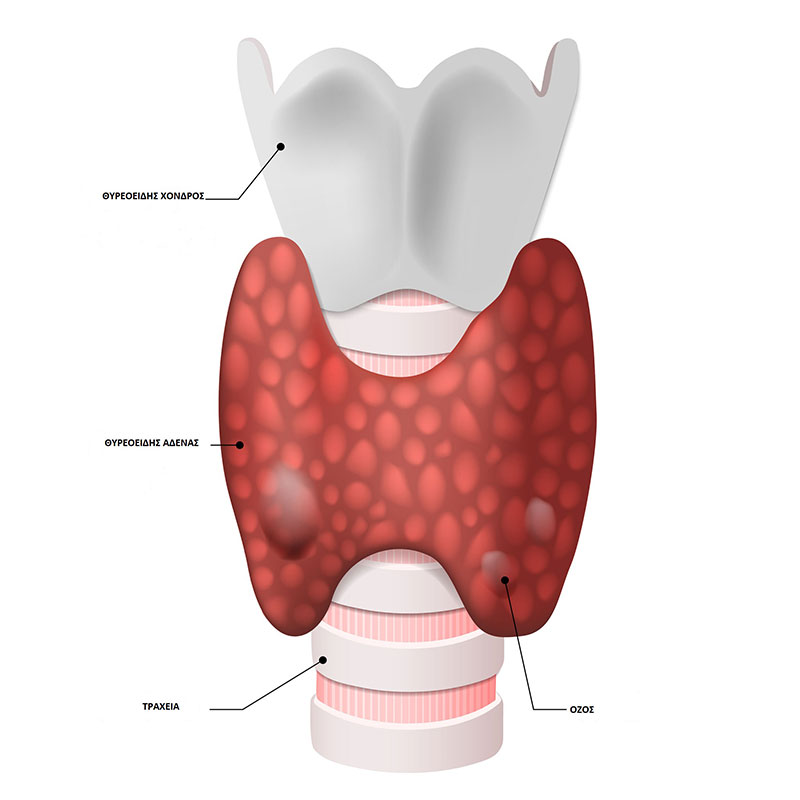
Thyroid cancer usually does not cause pain. However, if a thyroid mass is left and grows, it can cause swallowing and breathing problems, as well as hoarseness. In cases where bleeding occurs inside the tumor, there may be pain.
HOW THE DIAGNOSIS IS MADE
Initially, the doctor needs to get a detailed medical history and do a careful physical examination, especially of the thyroid gland. He then recommends some tests:
- Blood tests to measure hormones that control the function of the thyroid or produced by it (TSH, fT4, fT3). There are usually no hormonal abnormalities in thyroid cancer. But hormonal tests can show if there is hypothyroidism or hyperthyroidism.
- Cervical / thyroid ultrasonogram, which shows the shape and size of the thyroid, the presence, size and composition of the nodules as well as the possible presence of suspicious lymph nodes in the cervix.
- Scintiscan of the thyroid gland, which shows the shape, size and function of the gland and nodules. Thyroid cancer is usually depicted as a cold nodule (does not take up the radioisotope). In this way it can be proved whether a mass is a goiter or not. Thyroid scintiscan contributes substantially to the diagnosis of various abnormalities that manifest in this organ.
- Examination of the cells that make up a thyroid torulus, after fine needle aspiration (FNA) can give information whether it is cancer or not.
TYPES OF THYROID CANCER
There are basically 4 types of thyroid cancer:
- Papillary type: It constitutes 80% of the cases. It grows in thyroxine-producing cells. It can show frequent relapses. The cure rate is 90 to 95%.
- Follicular type: It grows in the same cells and also has a high cure rate, amounting to 75% at 5 years from diagnosis. It is more common in women. It can infiltrate the lymph nodes and has the ability to metastasize.
- Myeloid type: It constitutes 5% -10% of cases. It can metastasize. It secretes the hormone calcitonin. It can coexist with other cancers of the endocrine system. At 5 years the survival rate is 70% .
- Regenerative type: It occurs mainly in people over 65 years. It is the rarest form and the most dangerous of the thyroid cancers. It is evolving very fast, it is very aggressive. It quickly infiltrates local tissues, throat structures and causes respiratory problems.
TREATMENT
Surgery to remove thyroid cancer is the first treatment performed. Usually, a total thyroidectomy is performed, which ensures the cure of both benign and most cases of thyroid cancer. In some cases, the surrounding lymph nodes need to be cleansed. Most patients are then treated with radioactive iodine. Radioactive iodine is absorbed by the thyroid and destroys residual cancer cells.
Other therapeutic weapons that can be used include radiotherapy and hormone therapy. Thyroid cancers do not respond well to chemotherapy, although in rare cases it may be given.
Finally, all patients receive lifelong thyroxine replacement therapy as directed by the endocrinologist, who monitors the patient postoperatively.
 English
English  Ελληνικά
Ελληνικά