Onychomycosis is a contagious infection and is divided into the following types:
Peripheral onychomycosis, which affects the free edge of the nail but also the hyponychium, white superficial onychomycosis which affects the surface of the nail and total onychomycosis.
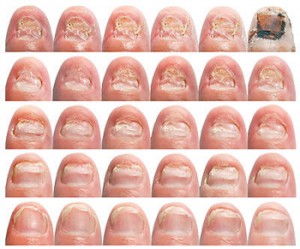
In peripheral onychomycosis, which is most common in toenails, the fungus first affects the stratum corneum of either the hyponychium or the lateral nail fold and then that of the nail bed. A mild inflammatory reaction is created, which leads to epidermis of the bed epithelium, creating a granular layer. Hyponychial hyperkeratosis forms, lifting of the nail plate from its bed, usually in the form of "channels" below it (onycholysis).
These conditions, as well as the secondary colonization by opportunistic fungi, lead to the change of the color of the nail (yellow to brown), to its fragility and to the loss of its gloss. The fungus then moves to the proximal part of the nail and eventually infects its uterus, infecting the newly formed nail, as well as more superficial layers and finally the entire nail plate.
The causes of onychomycosis
Predisposing factors for onychomycosis are arterial and venous disorders, recurrent injuries (eg in athletes), peripheral nerve disorders, diabetes mellitus, advanced age (40-50% of people are over 50 years old), immune disorders, psoriasis, nail length (free edge length over 3mm seems to favor the settlement of fungi and bacteria in the area under the nail), hyperhidrosis, fungal infections of the skin, deformity of the feet and toes (due to friction and moisture), lack of vitamins (A, B1, B2), excessive hygiene, use of common areas such as the swimming pool, etc.
The most common types of fungi
There are several types of fungi that affect the nails of the lower limbs. The most common species are:
on the fingernails the fungi of the genus Candida
on toenails mainly dermatophytes (Trichophytonrubrum)
Treatment given by the doctor
The diagnosis of onychomycosis is made by the competent doctor with the method of culture, because the clinical picture of the nail in a person with e.g. psoriasis or injury, in many cases is identical to the clinical picture of the nail with onychomycosis. An important element that the culture reveals is the type of fungus, which is needed for its successful treatment.
The degree of fungal infection in the nail is also crucial for the following treatment by the doctor, whether localized or systemic treatment will be done (combination of medication and localized treatment).
If a large number of nails or more than 50% of the nail plate is inffected, pure localized treatment does not bring satisfactory results.
The responsibilities of the podiatrist
The podiatrist meticulously removes from the fungus the affected part of the diseased nail plate. This procedure is necessary to clean the affected area and the doctor's medication works more effectively and should be repeated every 4-5 weeks until, with a new culture, the doctor determines that the area has been cleared of the fungus.
In addition to treating diseased nails, the podiatrist is responsible for advising his client on home care, which includes
Indication of the need for diligent nail care with special drugs, which are registered by the treating doctor
- The use of cotton or wool socks, which must be changed daily
- Using only leather, soft shoes
- The airing (even better the change) of shoes and their treatment with special consumables (sprays) to remove the fungus
- Avoid foot baths with very hot water. The foot baths should be done for a maximum of 3-5 minutes and the water should not exceed 35 ‘C
- Daily foot washing
- Good drying of the feet after washing, especially in the interdigital folds
- Τhe avoidance of common areas such as the swimming pool, etc.
Onychomycosis treatment is long-term and only the responsible and persistent cooperation of the sufferer can ensure the desired result which is the elimination of the fungus.
Source: doctoranytime.gr
 English
English  Ελληνικά
Ελληνικά